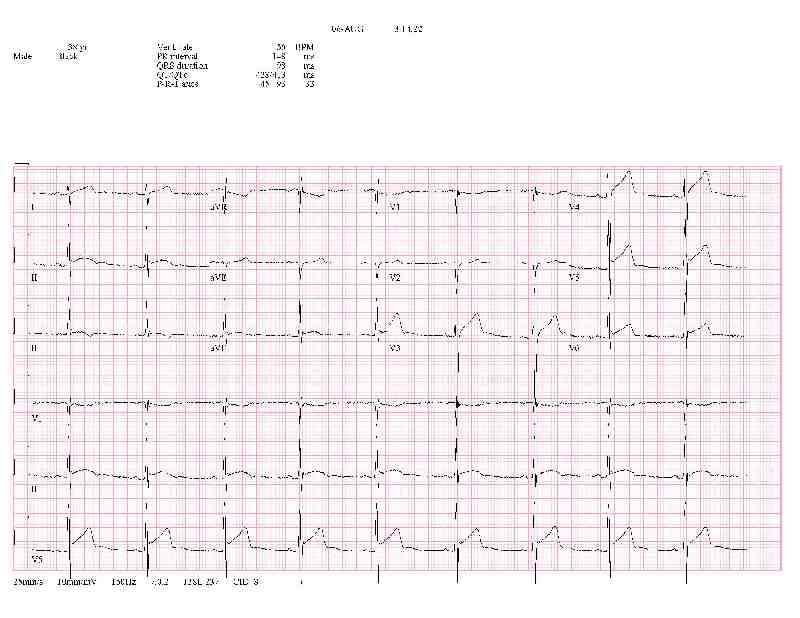
This 38 yo M with no PMH and no h/o of tobacco, alcohol, or drug abuse, presented complaining of one week of intermitted CP and SOB. He had the pain when I initially evaluated him, but it spontaneously remitted within minutes.
What is your diagnosis? What would you like to do?
Comments
This patient is a little young to be having an MI, especially considering there was no history of cocaine use (and the u-tox was negative).
Next, the initial EKG's, while concerning, are a little puzzling in that the abnormalities are not completely in an anatomic distribution, unless perhaps anterolateral or solely a lateral infarction (ST elevation in I, II, V3-V6, but then also in aVF?
Regardless, with an EKG like this you have to call it a STEMI, which I did. I called cardiology saying as much, and asked them to take the pt to the cath lab.
Cardiology was not entirely convinced. And based on the pt's clinical presentation (he didn't look like he was having a heart attack-- no current CP, SOB, diaphoresis, pallor, N/V), they ordered a STAT echocardiogram. That was basically normal but follow-up EKG's showing persistent abnormalities convinced them, and the pt went emergently to the cath lab.
The cath was negative except for slightly slowed flow in one of the branches of the circumflex or obtuse margninal, which might have been consistent with a small thrombus that passed. So the cath was diagnostic only (no stents placed, no balloon angioplasty performed, and no medications infused), and the pt was discharged from the post-procedure room. He only ever had one set of cardiac enzymes drawn and that was in the ED:
| Lab | Value |
|---|---|
| Troponin | < 0.02 |
| CK | 279 (0 - 200) |
| CKMB Mass | 1.7 |
The take home point is this: this EKG shows sufficient abnormalities that cardiology must be called for an emergent cath. Follow-up EKG's are always a good idea and should be obtained in equivocal cases, any time the pt's clinical condition (or symptoms) change, or after treatment.
Remember that EKG final reads are done by a cardiologist who may not know anything about the patient's presentation, course, or outcome. It is interesting to note that the first two EKG's were not read as an acute MI, the third and fourth ones were (20-30 minutes after the first EKG). It is also interesting to note that the EKG machine's reads were AMI for all four EKG's.
Do not rely solely on the machine's interpretation.