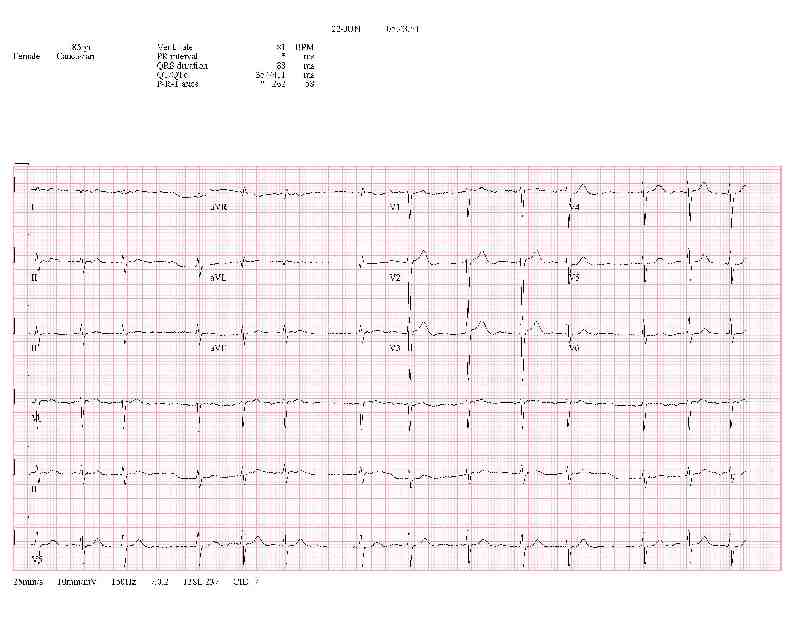
You can read the cardiologist's interpretation of each EKG above, but here are some
thoughts to help with the interpration.
If the are no P waves, but the QRS is narrow and irregular, the rhythm is most likely
atrial fibrillation. If the are no P waves, but the QRS is narrow and regular, the rhythm
is most likely junctional.
However, the rhythm here alterantes between being regular and irregular. So there must be
some reason that the AV node rate is not maintained. One possibility is that the AV node
is being overridden by a depolarization from above (sinus or atrial). Since there are no
P waves, and the rate of the overriding is irregular, the most likely choice is atrial
fibrillation.
So, there is either a severe electrolyte abnormality causing the absence of P waves
(like hyperkalemia, which is unlikely because the rate and QRS are normal) or atrial
fibrillation too fine to show up on the tracing. If there is atrial fibrillation,
why isn't the ventricular rate higher? Either there is a partial or intermittent block,
the atrial fibrillation waves are not of a high enough magnitude to depolarize the
AV node, or the patient is on a medicine such as diltiazem to control the ventricular
rate.
Note, when learning EKG's one might consider a wandering junctional pacemaker, akin to
a wandering atrial pacmaker, or multi-focal junctional tachycardia, akin to multi-focal
atrial tachycardia (MAT). However, neither of these entities exist, so the final diagnosis
is a junctional rhythm being intermittenly overridden ("competing with) atrial
fibrillation.
I do find it interesting that the cardiologist interpretations of the two EKG's differ
yet the second EKG was read as "No significant change". This underscores the fact that
the cardiologist may have more experience with cardiac issues, EKG's, and the like, but
he/she does not have the pt, and probably has no access to the chart, treatments,
electrolytes, x-rays, etc.
So, always read your own EKG's.