The pt was found to be in pulmonary edema, and was treated for such
PMH
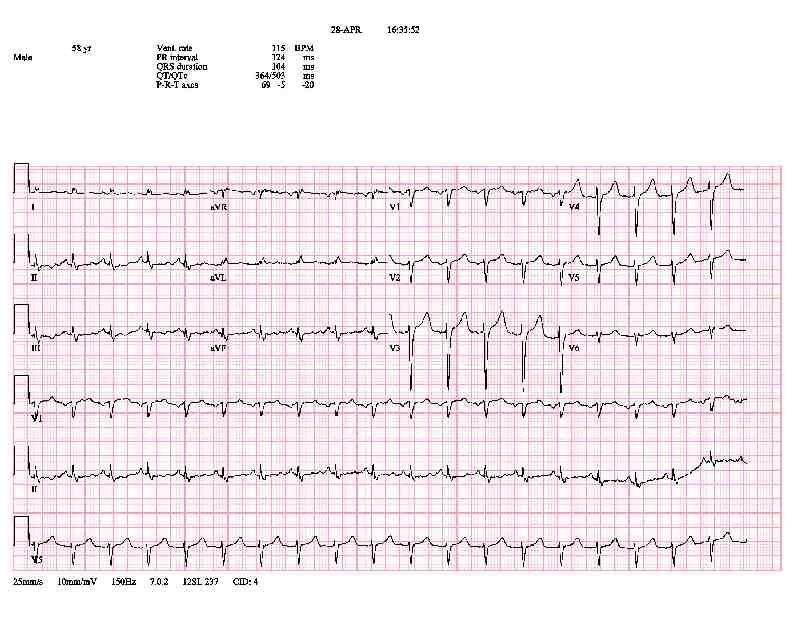
The pt presented with the following EKG. What would you like to do? What is your diagnosis?
The pt had an EKG from 7 weeks earlier when he presented with stabbing epigastric pain followed by acute shortness of breath.
The cardiologist noted that the incompleted LBBB is no longer present. However, more concerning is that the TWI's are no longer present (i.e. pseudonormalization). And the pt is tachycardic suggesting that something is wrong.
| Time | Troponin |
|---|---|
| Upon Presentation | 0.05 |
| When the EKG pseudonormalized | 5.52 |
| 4 days later | 0.88 |
At the first visit (the earlier EKG above), the pt was ruled-out for MI with three sets of troponins. A TTE showed an EF of 25% along with a foreign body in the right ventricle extending through to the outflow tract (confirmed by CT). The pt was offered operative repair (replacement) of his MV - and removal of the foreign body - which he refused saying he would rather go back to the hospital that did the initial repair.
At the second admission (the EKG above that showed pseudonormalization) the patient was intubated in the ED for respiratory distress, treated for pulmonary edema, and admitted to the CCU. The pt was extubated in the CCU, and a workup revelaed mitral regurgitation. He consented for a repeat mitral valve repair, was extubated on POD #2, and though he needed his chest tubes for an extended period of time due to continued draininage and suffered a thigh hematoma treated conservatively with warm compresses, he did well and ultimately left the hospital.